
Ever been in a snakebite situation where the victim needed immediate protection, not a month-long wait for immunity to develop? If you’re nodding, you already understand why sometimes we need passive immunity from sera, not vaccines.
Most of us only think about immunity when seasonal flu shots roll around or when travel requires vaccination paperwork. But the distinction between passive and active immunity can literally be life-or-death in emergency medicine scenarios.
Understanding the difference between passive vs active immunity isn’t just medical trivia—it’s practical knowledge that explains why doctors might reach for antibody-packed sera when a vaccine would be too slow to help. When your body needs borrowed antibodies right now instead of instructions to make its own, timing changes everything.
So what exactly happens in your bloodstream during these two immunity types? And when does each approach make the most sense?
Understanding Immune Responses: The Body’s Defense Mechanisms

How our immune system protects us
Your body is a battlefield every single day. Bacteria, viruses, fungi, and parasites constantly try to invade your personal space. But you’re not defenseless – far from it.
Your immune system is like a highly trained military with different specialized units. First up is your innate immune system – the bouncers at the club. These guys don’t care who you are; if you’re not supposed to be there, they’re throwing you out immediately. This includes physical barriers like your skin and mucous membranes, plus cellular defenders like neutrophils and macrophages that engulf invaders on sight.
Then there’s your adaptive immune system – the special forces that develop targeted attacks against specific threats. These teams remember previous invaders and launch faster, stronger responses when they see them again.
The stars of this show? B cells and T cells.
B cells are your weapons manufacturers, producing antibodies that stick to pathogens like targeted missiles, marking them for destruction. T cells come in different flavors – helper T cells coordinate the immune response while cytotoxic T cells directly eliminate infected cells.
And that’s just scratching the surface of this incredible defense network.
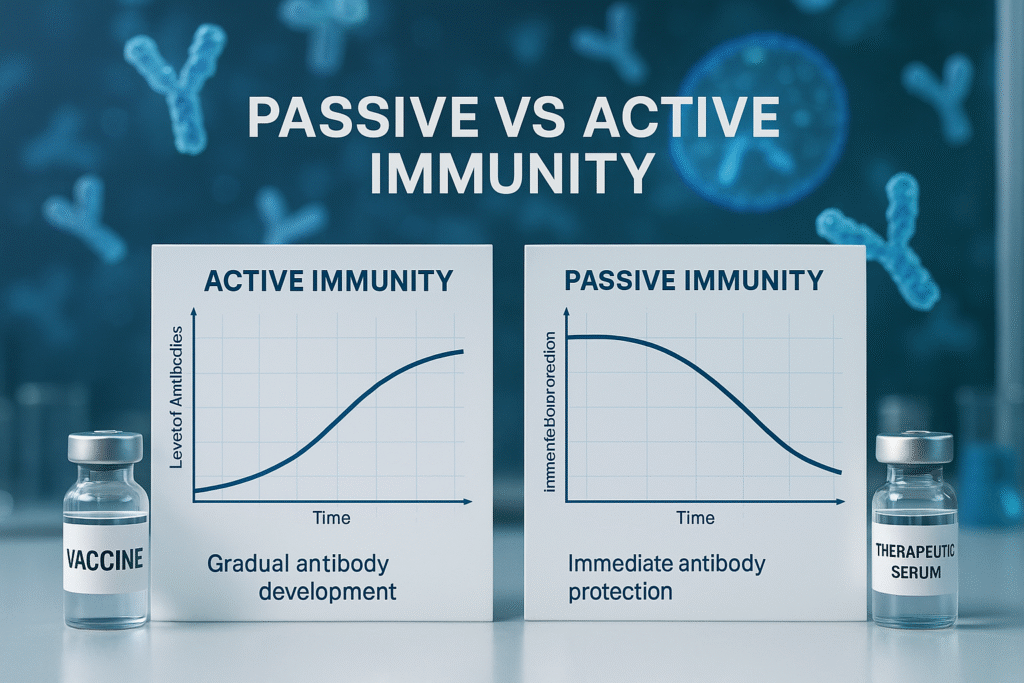
The critical difference between active and passive immunity
Active immunity is like learning to cook for yourself. It takes effort up front, but then you can feed yourself for life. When your body encounters a pathogen (or a vaccine that mimics one), it creates antibodies and memory cells specific to that threat. The process takes time but provides long-lasting protection.
Passive immunity? That’s like ordering takeout. You get immediate satisfaction without doing the work, but it doesn’t last. This happens when you receive pre-made antibodies produced by another person or animal.
Check out these key differences:
| Active Immunity | Passive Immunity |
|---|---|
| Self-produced antibodies | Received antibodies |
| Slow to develop (days/weeks) | Immediate protection |
| Long-lasting (years/lifetime) | Temporary (weeks/months) |
| Memory cells created | No memory cells |
| Examples: infection recovery, vaccines | Examples: maternal antibodies to newborns, immunoglobulin therapy |
Timeline of immunity development: Why timing matters
Immunity isn’t instant – it’s a process with distinct phases.
When your body first encounters a pathogen, there’s the “lag phase” where you have little to no protection. This can last 4-7 days while your immune system identifies the threat and mobilizes forces. During this time, you’re vulnerable – which is why passive immunity can be lifesaving in certain situations.
Next comes the “active response phase” where antibody levels rise dramatically as your B cells churn them out. This peaks around 10-14 days after exposure.
Finally, there’s the “memory phase” where antibody production decreases but memory B and T cells remain vigilant, ready to spring into action if the threat returns.
This timeline explains why you don’t get immediate protection from vaccines, but also why you can still get sick shortly after vaccination.
How memory cells create long-term protection
Memory cells are your immune system’s version of elephant memory – they never forget.
After fighting off an infection, most immune cells die off, but a small population of B and T memory cells persists, sometimes for decades. These cells hang out in your bone marrow and lymphatic tissues, like veterans telling war stories.
What makes them special is their ability to respond lightning-fast when they recognize a returning threat. Instead of the slow primary response that took days or weeks, memory cells trigger a secondary response within hours.
Memory B cells rapidly divide and produce high-affinity antibodies, while memory T cells quickly multiply and coordinate attacks. This rapid response often eliminates the threat before you even develop symptoms.
This memory response is why you typically only get diseases like chickenpox or measles once, and it’s the principle behind vaccination – training your memory cells without suffering through the actual disease.
Active Immunity: Building Your Body’s Defenses

A. Natural active immunity through infection
Ever caught a cold and noticed you didn’t catch the same one again right away? That’s natural active immunity at work. When germs invade your body, your immune system jumps into action like a well-trained army. It identifies the invader, creates specific antibodies to fight it, and remembers how to make those antibodies again if the same threat returns.
Think of it as your body’s way of taking notes during battle. After fighting off a virus like chickenpox, your immune system keeps a detailed playbook of how to defeat it. That’s why most people only get chickenpox once in their lifetime.
The process isn’t always pleasant though. The symptoms you experience during an illness—fever, inflammation, fatigue—are actually signs your immune system is hard at work building this protection.
B. Vaccine-induced active immunity: How vaccines train your immune system
Vaccines are basically a fire drill for your immune system. They contain weakened or inactivated parts of a pathogen—just enough to trigger an immune response without making you sick.
When you get vaccinated, your body encounters what looks like the real threat but without the danger. Your immune cells still create antibodies and memory cells, but you skip the whole “being sick” part. Pretty clever, right?
Different vaccines work in different ways:
| Vaccine Type | What It Contains | Examples |
|---|---|---|
| Live attenuated | Weakened version of the pathogen | MMR, chickenpox |
| Inactivated | Killed version of the pathogen | Polio, hepatitis A |
| Subunit/conjugate | Pieces of the pathogen | Hepatitis B, HPV |
| mRNA | Instructions for making a pathogen protein | Some COVID-19 vaccines |
C. Advantages of active immunity: Long-lasting protection
The biggest perk of active immunity? It sticks around. Whether you’ve recovered from an actual infection or received a vaccine, the protection typically lasts years—sometimes even a lifetime.
This durability comes from memory B and T cells that hang out in your body, ready to recognize and respond to threats they’ve seen before. They’re like veteran soldiers who can quickly mobilize and train new recruits when an old enemy appears.
Active immunity also gets stronger with repeat exposures. That’s why some vaccines require multiple doses or boosters—each exposure reinforces your immune memory and builds a more robust defense.
D. Limitations: Time required to develop protection
Active immunity isn’t instant. Your body needs time to recognize the threat, produce antibodies, and create memory cells. This process typically takes days or even weeks.
During this window, you remain vulnerable. That’s why getting vaccinated before flu season or before traveling to regions with specific disease risks is important—your body needs that head start.
Some vaccines require multiple doses spaced weeks or months apart to build full protection. The first dose introduces your immune system to the pathogen, while subsequent doses strengthen and extend the response.
E. Examples of successful vaccines and their impact on public health
Vaccines have transformed human health in ways our ancestors couldn’t imagine.
Smallpox—a disease that killed 300 million people in the 20th century alone—has been completely eradicated thanks to vaccination. Not a single natural case has occurred since 1977.
Polio has been eliminated from most countries worldwide. Before the vaccine, this disease paralyzed thousands of children every year in the US alone. Now we’re on the brink of global eradication.
Measles deaths have dropped by 73% globally since 2000 due to vaccination campaigns. That’s about 23 million lives saved in just two decades.
Vaccines prevent an estimated 2-3 million deaths annually across all age groups. Beyond saving lives, they’ve reduced disability, allowed children to attend school, and helped families avoid crushing medical expenses.
Passive Immunity: Borrowed Protection

Natural Passive Immunity: From Mother to Infant
Ever wonder why newborns don’t immediately catch every bug they encounter? Nature’s got a pretty sweet protection plan built in.
When a baby is still growing in the womb, mom’s antibodies cross the placenta and enter the baby’s bloodstream. These ready-made fighters start protecting the little one before they even take their first breath. IgG antibodies are the heroes here – they’re small enough to cross the placental barrier and give babies protection against the same things mom is immune to.
After birth, breastfeeding takes over as immunity central. The first milk (colostrum) is especially packed with antibodies – particularly IgA – that coat the baby’s digestive tract and respiratory system. These don’t enter the bloodstream but work like security guards at every entrance, blocking pathogens from setting up shop.
This borrowed protection is why breastfed babies typically get fewer infections in those crucial early months when their own immune systems are still figuring things out.
Artificial Passive Immunity Through Sera and Antibody Treatments
Sometimes we need a defensive boost, and we need it fast. That’s where therapeutic sera and antibody treatments come in.
Imagine you’ve been bitten by a venomous snake. Your body would eventually make antibodies against the venom, but that takes time you don’t have. An antivenom serum – containing pre-made antibodies from animals or humans who’ve developed immunity – gives you instant fighters to neutralize that poison.
Modern medicine has expanded this approach beyond just snake bites:
- Immune globulin therapy for patients with antibody deficiencies
- Monoclonal antibody treatments for certain cancers and autoimmune conditions
- Convalescent plasma from recovered patients during disease outbreaks
- Rabies immune globulin given after potential exposure
The beauty of these treatments? They work right away. No waiting around for your body to recognize the threat and mount a defense.
The Immediate Protection Advantage
Speed is the superpower of passive immunity. When you get antibodies directly:
- Protection begins within hours, not days or weeks
- No waiting for your immune system to recognize and respond
- Full protective levels immediately rather than gradually building up
- No need for multiple doses or boosters to reach protective levels
This makes passive immunity the go-to choice in crisis situations:
- After exposure to deadly diseases like rabies or tetanus
- During active infection when your immune system needs reinforcements
- For immunocompromised patients who can’t produce adequate antibodies
- In newborns facing specific infections before vaccination is possible
Why Passive Immunity Is Temporary
Here’s the catch – those borrowed antibodies don’t stick around forever.
Unlike your own immune cells that keep producing antibodies as needed, the ones you receive passively are like one-time visitors. They do their job, then gradually break down with no replacement team coming in. The borrowed antibodies have a half-life – typically a few weeks to a few months – before they degrade and disappear from circulation.
Your body also recognizes these foreign proteins as “not self,” so it slowly eliminates them. This explains why maternal antibodies protect babies for only about 6-12 months after birth, and why therapeutic sera treatments often need repeating.
The temporary nature also explains why we don’t just give everyone antibodies instead of vaccines. It would require constant treatments to maintain protection, making it both impractical and expensive as a long-term strategy.
This trade-off – immediate but temporary protection – is why passive immunity works best as a short-term solution while your body either recovers or develops its own active immunity through infection or vaccination.
Therapeutic Sera: Life-Saving Treatments

What Sera Contain: Antibodies Ready for Action
Ever wondered what’s actually in that syringe when a doctor administers therapeutic serum? It’s basically an antibody cocktail – ready-made immune soldiers that go to work immediately in your body.
Unlike vaccines that train your immune system to make its own antibodies (which takes time), sera contain fully-formed antibodies that someone or something else already made. These antibodies – also called immunoglobulins – are proteins specifically designed to recognize and neutralize threats like toxins, venoms, or pathogens.
The beauty of therapeutic sera is that they work right away. When you’re bitten by a venomous snake, you don’t have time to wait weeks for your body to build immunity. You need protection now, and that’s exactly what sera deliver.
These antibodies bind directly to their targets in your bloodstream, creating complexes that your body can safely eliminate. They’re like an elite tactical squad that swoops in when your body’s regular defenses aren’t prepared for the battle ahead.
How Therapeutic Sera Are Produced and Purified
The production of therapeutic sera isn’t for the squeamish. Most sera start with animals – typically horses or sheep – that are exposed to small, non-lethal amounts of the target toxin or pathogen. As these animals develop immunity, their blood becomes rich with protective antibodies.
Blood is collected from these immunized animals and goes through a separation process to isolate the liquid portion (serum) containing those precious antibodies. But raw serum isn’t ready for human use yet – it needs serious purification.
Modern purification techniques involve multiple steps:
- Fractionation to separate different protein components
- Enzyme treatments to break down unwanted proteins
- Filtration through special membranes
- Heat treatments to kill potential pathogens
- Chemical treatments to remove viruses
This purification is crucial because unpurified animal serum can cause severe allergic reactions in humans – the infamous “serum sickness” that was common in medicine’s earlier days.
Today’s therapeutic sera are highly refined products where most of the animal proteins have been removed, leaving primarily the therapeutic antibodies behind. Some newer sera are even produced using recombinant DNA technology or from human donors to reduce the risk of reactions.
Types of Sera Available for Medical Use
When it comes to therapeutic sera, doctors have several options depending on what they’re fighting:
Antivenom sera: The lifesavers you need after encounters with venomous snakes, scorpions, spiders, and marine creatures. Each antivenom is specific to particular species or families of venomous animals.
Antitoxin sera: These neutralize bacterial toxins from diseases like tetanus, botulism, and diphtheria. When these infections release their deadly toxins, antitoxins swoop in to neutralize them before they can cause harm.
Immune sera: Broader-spectrum products containing antibodies against specific infectious diseases. These might be used for diseases like rabies or hepatitis.
Human Immunoglobulin: Extracted from human blood donations, these products contain a mix of antibodies that reflect the donor population’s immunity. They’re used for everything from immune deficiencies to certain autoimmune conditions.
Success Stories: When Sera Saved Lives
The dramatic rescue stories involving therapeutic sera could fill volumes. Take the case of 10-year-old Aiden from Arizona, who was bitten by a rattlesnake during a hiking trip in 2023. Within minutes, his leg began swelling alarmingly, and pain shot through his body. Emergency airlift got him to a hospital where CroFab antivenom serum was administered. Within hours, the venom’s progress halted. By the next day, Aiden was stable – a stark contrast to what would have happened without this miracle medicine.
Or consider the botulism outbreak in Ohio in 2024, when contaminated home-canned vegetables affected seven people at a family gathering. The neurotoxin produced by Clostridium botulinum was rapidly paralyzing their respiratory muscles. Botulism antitoxin serum, rushed from strategic stockpiles, reversed the progression in five critically ill patients, preventing what would have otherwise been fatal outcomes.
Therapeutic sera don’t always make headlines, but they’re consistently saving lives in emergency rooms worldwide. When minutes count and the body has no time to develop its own defenses, these remarkable products bridge the gap between exposure and survival.
Clinical Decision Making: Vaccines vs. Sera

Emergency situations requiring immediate protection
When a patient shows up with a snake bite, there’s no time to wait for a vaccine to kick in. That’s the reality of emergency medicine where minutes matter.
Sera provide instant immunity in these life-or-death scenarios. Unlike vaccines that take days or weeks to generate protection, therapeutic sera deliver pre-formed antibodies that get to work immediately. Think of it as calling in reinforcements rather than training your own army.
Here’s when emergency sera is the clear choice:
- Snake bites or scorpion stings where venom is actively spreading
- Tetanus exposure in unvaccinated individuals with contaminated wounds
- Rabies exposure, especially with bites near the head where the virus can reach the brain quickly
- Botulism poisoning where toxins are already present
In emergency rooms worldwide, having these sera on hand can mean the difference between recovery and tragedy. The protection isn’t permanent, but when someone’s fighting for their life, lasting a few weeks is all that matters.
High-risk exposure scenarios: When time is critical
You’ve just been exposed to hepatitis A at that sketchy restaurant, or maybe your toddler picked up a used needle at the park. What now?
High-risk exposures create a race against time where post-exposure prophylaxis with sera often makes perfect sense. These situations demand protection before a pathogen gains a foothold.
Some classic scenarios include:
- Healthcare workers with needlestick injuries from patients with known hepatitis B
- Babies born to hepatitis B-positive mothers
- Close contacts of measles cases who aren’t immune
- Sexual assault victims with potential HIV exposure
The beauty of passive immunity in these cases is its immediacy. While a vaccine might eventually be part of the treatment plan, sera provides the bridge protection during that vulnerable window.
Immunocompromised patients: Special considerations
Cancer treatments, organ transplants, autoimmune disorders – all these conditions can leave the immune system too weak to respond properly to vaccines.
For these patients, sera might be the only realistic option for protection. Their compromised immune systems often can’t generate an adequate antibody response to vaccines, making passive immunity crucial.
Key situations include:
- Bone marrow transplant recipients exposed to varicella
- AIDS patients with severe immunosuppression
- Patients on high-dose steroids or biologics
- Individuals with primary immunodeficiency disorders
These patients need special consideration because their immunity resembles a broken shield – sera provides a temporary but functional replacement.
Outbreaks of rare but dangerous diseases
When unusual pathogens suddenly emerge, we often lack ready-made vaccines. Think Ebola, Marburg virus, or new strains of avian influenza.
During outbreaks of these rare but deadly diseases, sera from recovered patients has historically been a vital stopgap until vaccines can be developed. This approach was used extensively during the 2014 Ebola outbreak in West Africa.
The key advantages during outbreaks:
- No development time needed (antibodies are harvested from survivors)
- Immediate protection for healthcare workers and close contacts
- Targeted effectiveness against the specific strain causing the outbreak
Travel to endemic areas: Prevention strategies
Planning a last-minute trip to a region with high disease risk? Vaccines might not have enough time to generate protection before your departure.
For travelers heading to areas with yellow fever, hepatitis A, or other endemic diseases, sera can provide immediate short-term protection when vaccination timing isn’t ideal.
Smart travelers consider:
- Time before departure vs. vaccine activation period
- Risk level at the destination
- Duration of stay
- Existing immunity status
While vaccines remain the gold standard for travel preparation when time permits, sera serves as a critical backup option for those unexpected journeys that can’t wait for active immunity to develop.
Real-World Applications: When Sera Are the First Choice

A. Snake and scorpion envenomation: Racing against time
Ever been hiking and worried about what might be slithering or crawling nearby? That fear isn’t irrational. When someone gets bitten by a venomous snake or stung by a scorpion, every minute counts.
This is where antivenom sera shine. They’re the go-to treatment when there’s no time to wait for the body to build its own defense. Think about it – if you’re bitten by a cobra, your body would need weeks to develop antibodies, but the venom can kill within hours. Not exactly a fair race.
Antivenoms contain ready-made antibodies that immediately bind to venom molecules, neutralizing them before they can cause more damage. These antibodies come from animals (usually horses) that have been exposed to small amounts of venom and developed strong immune responses.
What makes antivenom treatment so critical is its speed. When properly administered, it can reverse symptoms within minutes to hours. For someone experiencing respiratory distress from a black mamba bite or cardiovascular collapse from a box jellyfish sting, that rapid response makes the difference between life and death.
B. Tetanus exposure in unvaccinated individuals
You step on a rusty nail. Ouch! If you’re up-to-date on your tetanus shots, you might just need a booster. But what if you’ve never been vaccinated or it’s been decades?
This is where tetanus immune globulin (TIG) comes into play. Doctors don’t mess around with tetanus – it has a mortality rate up to 30% even with modern treatment. The bacteria that cause tetanus, Clostridium tetani, produce a toxin so potent that even microscopic amounts can trigger the characteristic muscle spasms.
For unvaccinated people with contaminated wounds, waiting for a vaccine to kick in is gambling with their lives. Tetanus vaccines typically take at least two weeks to provide protection. The bacteria, meanwhile, could be producing toxins within hours.
TIG provides immediate protection by delivering antibodies that specifically target tetanus toxin. These antibodies get to work right away, buying time for the body while also getting vaccinated to develop long-term immunity.
C. Rabies post-exposure prophylaxis: Combining approaches
Rabies is brutal – nearly 100% fatal once symptoms appear. When someone gets bitten by a potentially rabid animal, doctors deploy a two-pronged strategy.
First comes rabies immune globulin (RIG), injected directly into and around the wound site. This delivers antibodies that immediately start neutralizing any rabies virus present. The goal? Stop the virus in its tracks before it reaches the nervous system.
Simultaneously, the person receives the first dose of rabies vaccine. Unlike the immune globulin, the vaccine stimulates the body to produce its own antibodies. It’s administered as a series of shots over two weeks to a month.
This combination approach exemplifies the perfect partnership between passive and active immunity. The sera provides immediate protection while the vaccine builds lasting defense.
D. Botulism and diphtheria: Neutralizing potent toxins
Botulism and diphtheria represent some of the most potent toxin-mediated diseases known to medicine. We’re talking about toxins so powerful that a microscopic amount can be deadly.
Botulism antitoxin is critical for neutralizing the nerve-blocking toxin produced by Clostridium botulinum bacteria. Whether from contaminated food, infected wounds, or intestinal colonization in infants, botulism toxin can cause progressive, descending paralysis that can eventually stop breathing.
Similarly, diphtheria antitoxin targets the toxin produced by Corynebacterium diphtheriae, which can cause a thick membrane to form in the throat and damage the heart, kidneys, and nervous system.
In both cases, vaccines exist but aren’t helpful after exposure. The toxins work too quickly, and the damage they cause is often irreversible. Antitoxin sera provide the only chance to intercept and neutralize these toxins before they bind to their targets in the body.
The window for effective treatment is narrow. For botulism, antitoxin is most effective when given within 24 hours of symptom onset. With diphtheria, earlier administration dramatically improves outcomes.
Future Developments in Immunity Management

Monoclonal antibody therapies: The next generation of passive immunity
Picture this: a world where we don’t just fight diseases reactively, but where we deploy perfectly engineered molecular soldiers programmed to target specific threats. That’s exactly what’s happening with monoclonal antibody therapies right now.
Unlike traditional sera that contain a mix of antibodies, monoclonal antibodies are precision-engineered clones that target one specific antigen. Think of them as special forces rather than a general army – they go after exactly what they’re trained to hit.
The COVID-19 pandemic pushed these therapies into the spotlight, but they’ve been quietly revolutionizing treatment for cancer, autoimmune disorders, and infectious diseases for years. Companies like Regeneron and Eli Lilly demonstrated how quickly these treatments could be developed when they rolled out COVID antibody cocktails in record time.
What makes them so exciting is their specificity. With traditional sera, you’re getting a shotgun approach – effective but messy. Monoclonal antibodies deliver sniper-like precision with fewer side effects. They’re the difference between carpet bombing and a surgical strike.
Extended half-life antibodies: Lengthening protection periods
One of the biggest drawbacks of passive immunity has always been its short duration. You get immediate protection, but it vanishes quickly – sometimes within weeks.
Scientists have cracked this problem by creating extended half-life antibodies. Through clever engineering tricks like Fc modifications and PEGylation, these super-antibodies stick around in your system much longer.
Some of these modified antibodies can provide protection for months instead of weeks. That’s a game-changer for conditions requiring ongoing treatment or for people in areas with limited healthcare access.
Take Nirsevimab, approved in 2023 for protecting infants against RSV. One dose provides protection for an entire RSV season – about 5 months. Before this innovation, monthly injections would have been necessary.
Combination approaches: Getting the best of both worlds
Why choose between active and passive immunity when you can have both? That’s the thinking behind combination approaches that are gaining traction.
Here’s how it works: passive antibodies provide immediate protection while vaccines kick-start your body’s own immune response. By the time the passive antibodies fade away, your active immunity is up and running.
This strategy is proving especially valuable for:
- Post-exposure prophylaxis for diseases like rabies
- Protecting immunocompromised patients who can’t mount strong responses to vaccines alone
- Fighting rapidly evolving pathogens where different angles of attack are needed
Emerging technologies in antibody engineering
The antibody engineering space is exploding with innovations that sound like science fiction:
Bispecific antibodies can grab two different targets simultaneously – like holding one bad guy with your left hand and another with your right. This approach is showing remarkable results in cancer immunotherapy.
Then there are antibody-drug conjugates (ADCs) that work like tiny guided missiles. The antibody finds the target, and the attached drug delivers the knockout punch exactly where needed.
Perhaps most fascinating are the programmable antibodies whose targeting can be adjusted as needed. Imagine a Swiss Army knife that can become exactly the tool you need at any moment.
While these technologies are primarily focused on treatment rather than prevention, they’re reshaping our understanding of how passive immunity can be leveraged against disease.
The immune system’s remarkable adaptability offers us different tools for different threats. Active immunity through vaccines provides long-term protection by training our bodies to recognize and fight specific pathogens, making it ideal for preventative healthcare. Meanwhile, passive immunity through therapeutic sera delivers immediate protection when time is critical, such as after exposure to venomous snake bites, rabies, or certain toxins. This dual approach to immunity management allows healthcare providers to select the most appropriate intervention based on urgency, patient condition, and the specific threat at hand.
As medical science advances, we can expect even more sophisticated immunity solutions that combine the immediate protection of sera with the lasting benefits of vaccines. For now, understanding the distinct roles of active and passive immunity helps us appreciate how these complementary approaches work together to save lives. Whether you’re receiving a routine vaccination or emergency sera treatment, both represent triumphs of medical science that continue to protect millions worldwide from infectious diseases and toxic exposures.

