
🦠 Imagine an enemy (Virus) so small, you can’t see it with the naked eye, yet so powerful it can bring the world to a standstill. This isn’t science fiction—it’s the reality of viruses, nature’s most enigmatic and formidable microscopic invaders.
From the common cold to global pandemics, viruses have been humanity’s constant, invisible companions throughout history. But how exactly do these tiny terrors manage to outsmart our sophisticated immune systems and wreak havoc on our bodies? It’s a tale of biological espionage, where viruses act as master manipulators, hijacking our cellular machinery for their own nefarious purposes.
In this deep dive into the world of viral infections, we’ll unravel the intricate dance between viruses and the human body. From their stealthy entry points to their cunning replication strategies, we’ll explore how these microscopic marauders manage to stay one step ahead of our defenses. Buckle up as we embark on a journey through the invisible battlefield within us, examining the viral invasion, our body’s counterattack, and the cutting-edge strategies scientists are developing to turn the tide in this ongoing biological war. 🔬💪
Understanding Viruses: Nature’s Microscopic Invaders

A. What are viruses and how do they differ from bacteria?
Viruses and bacteria are both microscopic organisms that can cause infections, but they have fundamental differences in structure, behavior, and impact on human health. Let’s explore these distinctions:
| Characteristic | Viruses | Bacteria |
|---|---|---|
| Size | Much smaller (20-400 nanometers) | Larger (0.2-10 micrometers) |
| Structure | Non-living, require host cells | Living organisms |
| Reproduction | Cannot reproduce independently | Can reproduce on their own |
| Cellular components | Lack cellular organelles | Have cellular structures |
| Genetic material | Only DNA or RNA | Both DNA and RNA |
| Antibiotic effectiveness | Not affected by antibiotics | Can be killed by antibiotics |
Viruses are essentially genetic material (DNA or RNA) encased in a protein coat, while bacteria are single-celled organisms with more complex structures. This fundamental difference impacts their behavior and interaction with host organisms.
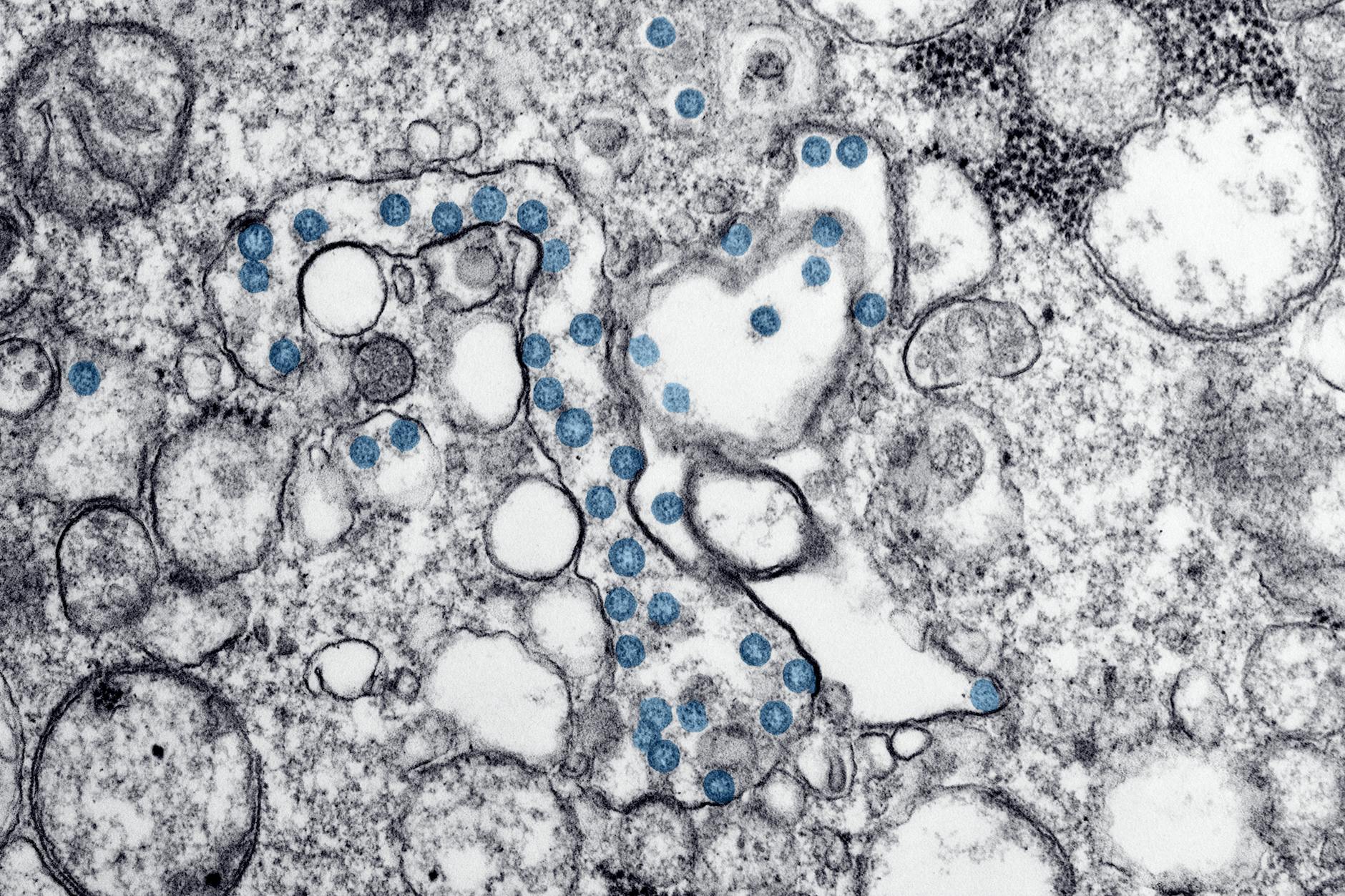
B. The structural components of a virus
A virus consists of several key components that enable its infectious nature:
- Genetic material: Either DNA or RNA, carrying the virus’s genetic code
- Capsid: A protein shell that encases and protects the genetic material
- Envelope (in some viruses): A lipid membrane surrounding the capsid
- Surface proteins: Specialized proteins that help the virus attach to host cells
The simplicity of viral structure belies its effectiveness in infiltrating and hijacking host cells. This streamlined design allows viruses to be highly adaptable and challenging to combat.
C. Types of viruses that affect humans
Viruses that infect humans can be categorized based on various factors, including their genetic material and structure. Some common types include:
- DNA viruses:
- Herpesviruses (e.g., HSV, EBV)
- Poxviruses (e.g., smallpox)
- Papillomaviruses (e.g., HPV)
- RNA viruses:
- Coronaviruses (e.g., SARS-CoV-2)
- Influenza viruses
- HIV (Human Immunodeficiency Virus)
- Retroviruses:
- HIV
- HTLV (Human T-cell Lymphotropic Virus)
- Hepatitis viruses:
- Hepatitis A, B, C, D, and E
Each type of virus has unique characteristics that influence its transmission, infection process, and impact on human health.
D. How viruses spread and infect new hosts
Viruses employ various strategies to spread and infect new hosts:
- Respiratory transmission: Through droplets or aerosols (e.g., influenza, COVID-19)
- Direct contact: Physical contact with infected individuals or contaminated surfaces
- Bloodborne transmission: Via blood or other bodily fluids (e.g., HIV, hepatitis B)
- Foodborne and waterborne: Contaminated food or water (e.g., norovirus, hepatitis A)
- Vector-borne: Transmitted by insects or other animals (e.g., Zika virus, West Nile virus)
Understanding these transmission routes is crucial for developing effective prevention strategies and controlling viral outbreaks. Public health measures, such as hand hygiene, vaccination programs, and vector control, play vital roles in limiting viral spread.
As we delve deeper into the world of viruses, we’ll next explore how these microscopic invaders enter the human body and begin their infectious cycle.
The Viral Invasion: Entering the Human Body

Common entry points for viruses
Viruses are opportunistic invaders that exploit various entry points in the human body to initiate infection. The most common entry points include:
- Respiratory tract
- Gastrointestinal tract
- Skin
- Mucous membranes
- Bloodstream
Let’s explore these entry points in more detail:
| Entry Point | Examples of Viruses | Transmission Method |
|---|---|---|
| Respiratory tract | Influenza, SARS-CoV-2, Rhinovirus | Inhalation of respiratory droplets |
| Gastrointestinal tract | Norovirus, Rotavirus | Ingestion of contaminated food or water |
| Skin | Papillomavirus, Herpes simplex | Direct contact with infected individuals or surfaces |
| Mucous membranes | HIV, Zika virus | Sexual contact, blood transfusions |
| Bloodstream | West Nile virus, Dengue virus | Insect bites (mosquitoes) |
How viruses bypass the body’s initial defenses
Once a virus reaches an entry point, it must overcome the body’s initial defense mechanisms. These defenses include:
- Physical barriers (skin, mucus)
- Chemical barriers (stomach acid, enzymes)
- Innate immune responses (interferons, natural killer cells)
Viruses employ various strategies to bypass these defenses:
- Mucus penetration: Some viruses secrete enzymes that break down mucus, allowing them to reach the underlying cells.
- pH resistance: Certain viruses have evolved to withstand the acidic environment of the stomach.
- Rapid replication: By multiplying quickly, viruses can overwhelm the initial immune response.
- Immune evasion: Some viruses can suppress or avoid detection by the innate immune system.
The role of receptor proteins in viral entry
After bypassing initial defenses, viruses must interact with specific receptor proteins on the surface of host cells to gain entry. This process involves:
- Recognition: The virus identifies and binds to a specific receptor protein on the cell surface.
- Attachment: Viral proteins form a strong bond with the receptor protein.
- Fusion or endocytosis: Depending on the virus type, it either fuses with the cell membrane or is engulfed by the cell.
Different viruses target different receptor proteins, which often determines their tissue tropism (preference for specific cell types). For example:
- Influenza virus targets sialic acid receptors in the respiratory tract
- HIV binds to CD4 receptors on T cells and macrophages
- SARS-CoV-2 uses ACE2 receptors found in various tissues
Understanding the interaction between viral proteins and cellular receptors is crucial for developing targeted antiviral therapies and vaccines. By blocking these interactions, we can prevent viral entry and potentially stop infections before they begin.
Now that we’ve explored how viruses enter the human body, we’ll delve into the next crucial step in viral infection: how these microscopic invaders hijack our cellular machinery to replicate and spread.
Hijacking Cell Machinery: Virus Replication

How viruses commandeer host cell resources
Viruses are master hijackers, expertly manipulating cellular machinery to their advantage. Upon entering a host cell, they immediately begin to take control of various cellular components, redirecting them towards viral replication. This process is both intricate and efficient, allowing viruses to rapidly multiply within the host.
Key resources that viruses commandeer include:
- Ribosomes
- Endoplasmic reticulum
- Golgi apparatus
- Mitochondria
- Nuclear pores
| Cellular Component | Normal Function | Viral Hijacking Purpose |
|---|---|---|
| Ribosomes | Protein synthesis | Production of viral proteins |
| Endoplasmic reticulum | Protein folding and transport | Assembly of viral particles |
| Golgi apparatus | Protein modification and sorting | Modification of viral proteins |
| Mitochondria | Energy production | Increased energy for viral replication |
| Nuclear pores | Controlled nuclear-cytoplasmic transport | Facilitation of viral genome entry/exit |
The viral replication cycle explained
The viral replication cycle is a multi-step process that allows viruses to reproduce rapidly within host cells. This cycle typically consists of the following stages:
- Attachment: The virus binds to specific receptors on the host cell surface.
- Entry: The virus penetrates the cell membrane and enters the cytoplasm.
- Uncoating: The viral genome is released from its protective capsid.
- Replication: The viral genome is copied using host cell machinery.
- Assembly: New viral particles are assembled from newly synthesized components.
- Release: Mature virus particles exit the cell, often causing cell lysis.
Speed and efficiency of viral reproduction
Viruses are incredibly efficient at reproducing, with some capable of generating thousands of new viral particles within a single host cell in just a few hours. This rapid reproduction rate is due to several factors:
- Streamlined genomes: Viruses have compact genetic material, allowing for quick replication.
- Hijacked cellular machinery: By using host resources, viruses avoid the need for their own complex replication systems.
- Parallel processing: Multiple stages of replication can occur simultaneously within a single cell.
- Efficient packaging: Viral genomes are designed for optimal assembly into new particles.
Why human cells can’t easily stop the process
Human cells face significant challenges in halting viral replication for several reasons:
- Molecular mimicry: Viruses often produce proteins that closely resemble host cell molecules, making detection difficult.
- Rapid mutation: Viruses can quickly evolve to evade cellular defenses.
- Interference with cellular signaling: Some viruses disrupt the cell’s ability to signal for help from the immune system.
- Overwhelming speed: The rapid replication of viruses can outpace the cell’s defensive responses.
- Cellular dependency: Infected cells may become reliant on viral proteins for survival, making it difficult to eliminate the virus without harming the cell.
Understanding these mechanisms is crucial for developing effective antiviral strategies. By targeting specific stages of the viral replication cycle or bolstering cellular defenses, researchers hope to create more potent treatments against viral infections. As we delve deeper into the complexities of viral tactics, we’ll explore how these microscopic invaders manage to evade detection by our immune system.
Immune System Response: The Body Fights Back

A. Recognizing viral invaders
The human immune system is a sophisticated network of cells, tissues, and organs that work together to defend the body against harmful pathogens, including viruses. The first step in mounting an effective immune response is recognizing the presence of viral invaders. This process involves several key components:
- Pattern Recognition Receptors (PRRs)
- Toll-like Receptors (TLRs)
- RIG-I-like Receptors (RLRs)
- NOD-like Receptors (NLRs)
These receptors are capable of detecting specific molecular patterns associated with viruses, known as Pathogen-Associated Molecular Patterns (PAMPs). Once a viral PAMP is detected, it triggers a cascade of immune responses.
| Receptor Type | Location | Viral PAMPs Detected |
|---|---|---|
| TLRs | Cell surface and endosomes | Viral nucleic acids, proteins |
| RLRs | Cytoplasm | Viral RNA |
| NLRs | Cytoplasm | Various viral components |
B. Innate immune responses to viral infections
The innate immune system provides the first line of defense against viral infections. It responds quickly but non-specifically to viral threats. Key components of the innate immune response include:
- Interferons (IFNs): These proteins are produced by infected cells and nearby uninfected cells. They interfere with viral replication and enhance the antiviral state of surrounding cells.
- Natural Killer (NK) cells: These cells recognize and destroy virus-infected cells without prior sensitization.
- Complement system: This group of proteins works together to identify and eliminate infected cells.
- Inflammatory response: This process recruits immune cells to the site of infection and helps contain the spread of the virus.
C. Adaptive immunity and virus-specific antibodies
While the innate immune system provides immediate protection, the adaptive immune system takes longer to develop but offers more targeted and long-lasting defense. Key components include:
- T cells: These cells can directly kill infected cells (cytotoxic T cells) or help coordinate the immune response (helper T cells).
- B cells: These cells produce virus-specific antibodies that can neutralize viruses or mark them for destruction by other immune cells.
- Memory cells: Both T and B cells can form memory cells, allowing for a faster and more robust response to future infections by the same virus.
D. The race between virus replication and immune response
The outcome of a viral infection often depends on the speed and effectiveness of the immune response relative to the rate of viral replication. This race is influenced by several factors:
- Viral replication rate
- Effectiveness of innate immune responses
- Speed of adaptive immune activation
- Pre-existing immunity from previous infections or vaccinations
E. Why some viruses are harder to fight than others
Some viruses pose greater challenges to the immune system due to various factors:
- Rapid mutation: Viruses like influenza can quickly change their surface proteins, making it difficult for the immune system to recognize them.
- Immune evasion tactics: Some viruses, such as HIV, have evolved mechanisms to avoid detection or suppress immune responses.
- Latency: Viruses like herpes simplex can remain dormant in the body, evading immune detection until they reactivate.
- Antigenic diversity: Some viruses, like rhinoviruses (common cold), have many different strains, making it challenging for the immune system to develop comprehensive protection.
Understanding these challenges is crucial for developing effective antiviral strategies and vaccines to combat persistent viral threats.
Viral Tactics for Evading Detection

Antigenic drift and shift
Viruses are masters of disguise, constantly evolving to outsmart our immune system. Two primary mechanisms they employ are antigenic drift and antigenic shift. These tactics allow viruses to evade detection and continue their infectious spread.
Antigenic drift
Antigenic drift refers to small, gradual changes in the surface proteins of viruses. These mutations occur naturally during viral replication and can accumulate over time. As a result, the virus’s appearance to the immune system changes slightly, making it harder for antibodies to recognize and neutralize the pathogen.
For example, influenza viruses undergo antigenic drift regularly, which is why we need annual flu shots. The table below illustrates the impact of antigenic drift on vaccine effectiveness:
| Time since vaccination | Vaccine effectiveness |
|---|---|
| 0-3 months | 70-90% |
| 3-6 months | 50-70% |
| 6-12 months | 30-50% |
| >12 months | <30% |
Antigenic shift
Antigenic shift, on the other hand, involves more dramatic changes in viral structure. This phenomenon occurs when two or more different strains of a virus infect the same host cell and exchange genetic material. The resulting hybrid virus can have entirely new surface proteins, rendering existing immunity ineffective.
Antigenic shift is less common but can lead to pandemic outbreaks, as seen with the 2009 H1N1 swine flu. The novel combination of genes created a virus that human immune systems had never encountered before.
Latency and viral dormancy
Another cunning tactic employed by viruses is the ability to enter a state of latency or dormancy within host cells. During this period, the virus remains inactive and undetectable by the immune system. This strategy allows viruses to:
- Persist in the body for extended periods
- Avoid immune detection and clearance
- Reactivate when conditions are favorable
- Cause recurrent infections
Examples of viruses that utilize latency include:
- Herpes simplex virus (HSV)
- Varicella-zoster virus (causes chickenpox and shingles)
- Human immunodeficiency virus (HIV)
Interfering with immune system signaling
Viruses have also developed sophisticated methods to disrupt the communication networks of our immune system. By interfering with signaling pathways, they can delay or prevent an effective immune response. Some common tactics include:
- Blocking interferon production: Interferons are crucial signaling molecules that alert nearby cells to the presence of a viral infection. Some viruses can inhibit interferon production, effectively silencing the alarm.
- Mimicking host proteins: Certain viruses produce proteins that closely resemble our own immune signaling molecules. This molecular mimicry can confuse the immune system and prevent it from mounting an appropriate response.
- Downregulating antigen presentation: Viruses can interfere with the process of antigen presentation, making it harder for immune cells to recognize infected cells.
- Inducing immunosuppressive cytokines: Some viruses stimulate the production of cytokines that suppress immune function, creating a more favorable environment for viral replication.
By employing these evasion tactics, viruses can establish long-lasting infections and cause significant damage to the host. Understanding these mechanisms is crucial for developing more effective antiviral treatments and vaccines. As we continue to unravel the complexities of viral evasion, we can better equip ourselves to combat these microscopic invaders and protect human health.
The Impact of Viral Infections on Human Health
Short-term effects: common symptoms and why they occur
When a viral infection takes hold, our bodies often respond with a range of common symptoms. These symptoms are actually the result of our immune system’s efforts to combat the invading virus. Let’s explore some of the most frequent short-term effects and their underlying causes:
- Fever
- Fatigue
- Muscle aches
- Cough and congestion
- Nausea and vomiting
Fever is perhaps the most recognizable symptom of viral infections. It occurs when the body raises its internal temperature to create an inhospitable environment for the virus. This elevated temperature also helps activate immune cells, accelerating their response to the infection.
Fatigue and muscle aches are often experienced together. These symptoms arise from the body’s reallocation of energy resources towards fighting the infection. Additionally, the immune response triggers the release of cytokines, which can cause inflammation and contribute to the sensation of muscle soreness.
Respiratory symptoms like cough and congestion are common in many viral infections, especially those affecting the respiratory tract. These symptoms are the body’s attempt to expel the virus and infected cells from the airways.
| Symptom | Cause | Purpose |
|---|---|---|
| Fever | Elevated body temperature | Create hostile environment for virus, activate immune cells |
| Fatigue | Energy reallocation | Direct resources to immune response |
| Muscle aches | Cytokine release | Signal immune activation, combat virus spread |
| Cough | Airway irritation | Expel virus and infected cells |
| Congestion | Mucus production | Trap and remove viral particles |
Long-term consequences of viral infections
While most viral infections resolve within days or weeks, some can lead to long-lasting health issues. These long-term consequences can vary widely depending on the specific virus and the individual’s overall health. Some notable examples include:
- Post-viral fatigue syndrome
- Organ damage
- Neurological complications
- Increased risk of autoimmune disorders
- Persistent inflammation
Post-viral fatigue syndrome, sometimes referred to as chronic fatigue syndrome, can occur after severe viral infections. Patients may experience prolonged periods of exhaustion, cognitive difficulties, and muscle weakness that persist long after the initial infection has cleared.
Certain viruses can cause lasting damage to organs such as the heart, lungs, or liver. For instance, viral myocarditis can lead to long-term heart complications, while severe respiratory viruses may result in reduced lung function even after recovery.
Neurological complications are another potential long-term consequence of viral infections. Some viruses can directly affect the nervous system, leading to issues like persistent headaches, memory problems, or even more severe conditions such as encephalitis or Guillain-Barré syndrome.
Chronic viral infections and their management
Some viruses have the ability to establish long-term, persistent infections within the body. These chronic viral infections require ongoing management and can significantly impact an individual’s health over time. Examples of chronic viral infections include:
- HIV/AIDS
- Hepatitis B and C
- Herpes simplex virus (HSV)
- Human papillomavirus (HPV)
- Epstein-Barr virus (EBV)
Managing chronic viral infections often involves a combination of antiviral medications, immune system support, and lifestyle modifications. The primary goals of management are to:
- Suppress viral replication
- Prevent disease progression
- Minimize transmission risk
- Manage symptoms and complications
For instance, in the case of HIV, antiretroviral therapy (ART) is used to keep the virus suppressed, allowing patients to lead relatively normal lives and significantly reducing the risk of transmission to others. Similarly, chronic hepatitis B and C infections are managed with antiviral medications to prevent liver damage and reduce the risk of liver cancer.
Regular monitoring is crucial in the management of chronic viral infections. This may include blood tests to check viral load, assess organ function, and monitor for potential complications. Additionally, patients with chronic viral infections often benefit from a holistic approach that includes proper nutrition, stress management, and mental health support.
As we’ve seen, viral infections can have a wide range of impacts on human health, from short-term symptoms to long-lasting consequences and chronic conditions. Understanding these effects is crucial for developing effective prevention strategies and treatment approaches. In the next section, we’ll explore some of the cutting-edge antiviral strategies that researchers are developing to combat these microscopic invaders.
Cutting-Edge Antiviral Strategies

Vaccines: Training the body to recognize viruses
Vaccines represent one of the most effective antiviral strategies, training our immune system to recognize and combat specific viruses before they can cause harm. This proactive approach has revolutionized our ability to prevent viral infections and save millions of lives.
How vaccines work
Vaccines work by introducing a harmless version of the virus or its components to our immune system. This process stimulates the production of antibodies and memory cells, creating a robust defense mechanism. Here’s a simplified breakdown of the vaccine process:
- Introduction of viral antigens
- Immune system recognition
- Antibody production
- Memory cell formation
- Long-term protection
| Vaccine Type | Description | Examples |
|---|---|---|
| Live attenuated | Weakened form of the virus | MMR, Chickenpox |
| Inactivated | Killed virus | Polio, Flu shot |
| Subunit | Specific parts of the virus | Hepatitis B |
| mRNA | Genetic instructions for virus proteins | COVID-19 (Pfizer, Moderna) |
Antiviral medications and how they work
While vaccines prevent infections, antiviral medications treat existing viral infections. These drugs target various stages of the viral life cycle to inhibit replication and spread.
Common antiviral mechanisms:
- Blocking viral entry into cells
- Inhibiting viral enzyme activity
- Interfering with viral genetic material replication
- Preventing virus assembly or release
Antiviral medications have proven crucial in managing infections like HIV, influenza, and herpes. However, the development of new antivirals remains challenging due to viral mutations and drug resistance.
Gene editing techniques to combat viral infections
Emerging gene editing technologies, such as CRISPR-Cas9, offer promising avenues for antiviral strategies. These techniques allow scientists to modify genetic material with unprecedented precision, potentially enabling us to:
- Disable viral genes essential for replication
- Enhance cellular resistance to viral infection
- Correct genetic vulnerabilities that make individuals susceptible to certain viruses
While still in experimental stages, gene editing approaches could revolutionize our ability to combat viral infections at the genetic level.
The potential of immunotherapy in treating viral diseases
Immunotherapy, traditionally associated with cancer treatment, is now being explored as a powerful tool against viral infections. This approach harnesses the body’s immune system to fight viruses more effectively.
Immunotherapy strategies for viral infections:
- Monoclonal antibodies: Lab-created antibodies that target specific viral proteins
- Adoptive T cell therapy: Engineering T cells to recognize and destroy virus-infected cells
- Cytokine therapy: Boosting the immune response with synthetic immune signaling molecules
These cutting-edge antiviral strategies represent the forefront of our battle against viral infections. As we continue to unlock the secrets of viral biology and human immunity, we can expect even more innovative approaches to emerge, strengthening our arsenal against these microscopic invaders.

Viruses are remarkable in their ability to infiltrate our bodies and manipulate our cellular machinery for their own benefit. From their initial entry to their complex replication processes, these microscopic invaders pose a significant challenge to human health. Our immune system, though robust, often struggles to keep pace with the ever-evolving viral tactics for evading detection and continuing their spread.
As we continue to face viral threats, it’s crucial to stay informed and proactive about our health. Advancements in antiviral strategies offer hope for better prevention and treatment options. By understanding how viruses operate, we can better appreciate the importance of public health measures and support ongoing research efforts to combat these invisible enemies.

